How do we treat proliferative diabetic retinopathy?
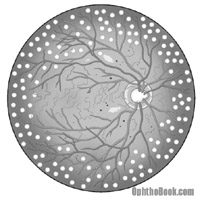 Proliferative retinopathy can be tricky to manage. Most of these patients seem to present because of symptoms, in many cases from vitreous hemorrhage from bleeding neovascular vessels at the optic nerve or elsewhere in the retina. If possible, the goal is to perform PRP (pan retinal photocoagulation) laser in the peripheral retina. This sacrifices peripheral retina, decreases VEGF production, and hopefully will cause the new vessels to regress.
Proliferative retinopathy can be tricky to manage. Most of these patients seem to present because of symptoms, in many cases from vitreous hemorrhage from bleeding neovascular vessels at the optic nerve or elsewhere in the retina. If possible, the goal is to perform PRP (pan retinal photocoagulation) laser in the peripheral retina. This sacrifices peripheral retina, decreases VEGF production, and hopefully will cause the new vessels to regress.
If there is too much blood to laser, however, then you wait until it does settle. If this is taking too long (several months) then you can consider taking the patient to surgery for a PPV (pars plana vitrectomy) with blood washout and endolaser.
Neovascularization of the iris is very difficult to treat … these patients develop acute glaucoma from new vessels clogging the trabecular meshwork. Perform PRP if you can see through the hazy cornea, otherwise aggressive pressure control is the key and the patient will likely need a tube-shunt placement.