Chapter 1: Eye history and physical
A thorough eye exam is important! Not only is the eye the most important organ in the body (of course!), but many common systemic diseases show ocular involvement. In fact, some conditions, like diabetes, may be first detected with the eye exam.
To help organize your eye exam, I’ve made a sample ophthalmology note on the facing page. Our clinic notes are difficult to interpret as our physical exam is long, specific, and requires many abbreviations to fit on a single page. Basically, it’s a combination of a neurology and a dermatology note. Here’s a rundown of the basic ophthalmology note’s components.
History of Present Illness:
As with all other specialties, a detailed ocular history is crucial to diagnosis. You should explore every complaint with the “basic questions” — when did it start, what’s it like, is there anything that makes it better or worse, are you taking any medications for relieve, etc..
Specific HPI review of systems should also include:
- Floaters and flashing lights: These are the classic symptoms of a retinal detachment and retinal tears so ask EVERY patient about these symptoms. Most patients complain of some floaters – see if they’re actually new or have worsened recently.
- Transient vision loss: Think of migraine vessel spasm in the young and micro-emboli in the elderly. Curtains of darkness might indicate an ischemic event or a retinal detachment, so explore these symptoms in detail.
- Blurry vision: Is the vision always blurry? Does it worsen when reading or watching TV (people blink less when watching TV and develop dry eyes). Is this a glare problem at night that might indicate cataracts? Does the diabetic patient have poor control and hyperglycemic swelling of the lens?
- Red, painful eyes: A common complaint. Be sure to ask about the nature of the pain (is this a scratchy pain, aching pain, or only pain with bright light). Is there discharge that might indicate an infection?
- Chronic itching and tearing: Think about allergies or blepharitis. Is it in both eyes?
- Headaches and scalp tenderness: Think of temporal (giant cell) arteritis and ask about other collaborating symptoms like jaw claudication, polymyalgias, weight loss, and night sweats.
The “Right Hand Column”
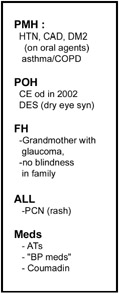
PMH (past medical history):
Past medical history should include the usual health questions, but with the main emphasis on conditions directly contributing to ocular pathology such as diabetes, hypertension, and coronary artery disease. Also, ask about thyroid problems and asthma (you might need to prescribe a beta-blocker and you don’t want to set off bronchospasm).
POH (past ocular history):
Ocular history should inquire about past clinic visits and surgeries. Specifically inquire about cataract surgeries, eye trauma, and glaucoma. You can often piece together your patient’s ocular history by examining their eyedrops.
Family History:
Focus on history of glaucoma and blindness. Patients will often confuse glaucoma with cataracts, so be sure to clarify the difference.
Allergies:
List basic allergies and their reaction. We sometimes give Diamox to control eye pressure so make sure your glaucoma patient isn’t allergic to sulfa drugs.
Medications:
Find out what eyedrops your patient is taking, and why. Are they using a regular eyedrop? How about vasoconstricting Visine? Did they bring their drops with them? If your patient can’t remember their medications, it often helps to ask about the bottlecap-color of their drops (ex. all dilating drops have red caps). Also, it’s nice to know if your patient is taking an oral beta-blocker already, in case you want to start a beta-blocking eyedrop.
Vision, Pupil, and Pressure … oh my!
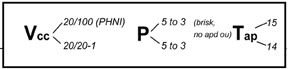 Vision, pupil, and pressure are the “vital signs” of ophthalmology. After a brief history, I check these measurements before dilating the eyes. This is because dilating drops will effect vision, pupil size, and potentially elevate our pressure measurements so you need to check these signs first. If you ever consult ophthalmology, we will always ask you …
Vision, pupil, and pressure are the “vital signs” of ophthalmology. After a brief history, I check these measurements before dilating the eyes. This is because dilating drops will effect vision, pupil size, and potentially elevate our pressure measurements so you need to check these signs first. If you ever consult ophthalmology, we will always ask you …
What’s the vision, pupil, and pressure?
It’s kind of a mantra. I don’t know how many times I’ve been told to “get the vision, pupil, and pressure, then dilate them.”
Visual Acuity:

You measure visual acuity with a standard Snellen letter chart (the chart with the BIG E on it). If your patient can’t read the E on the top line, see if they can count fingers at different distances. Failing this, try hand motion and light. Poor distance vision usually occurs from refractive error (your patient needs better glasses).
You want to check a patient’s “best corrected vision” so have them wear their glasses. You’re going to be amazed at the number of people complaining of “blurry vision” who leave their glasses in their car. You’ll also be impressed by the number of consults you’ll get where the consulting doctor hasn’t bothered to check the patient’s vision. Remember: “I can’t see!” is a relative complaint – for some this means 20/25 vision and for others this means complete darkness.
Das Pinhole!
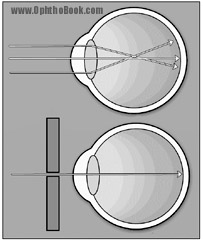 A quick and easy way to determine whether refraction is the culprit, short of actually testing different lenses, is with the pinhole test. Punch a small hole in a paper card, and have your patient reread the eye-chart while looking through this pinhole. This can actually improve vision by several diopters. It works because the paper blocks most of the misaligned rays that cause visual blur, and allows the central rays to focus on the retina. If your patient shows no improvement with pinholing, start thinking about other visual impediments like cataracts or other media opacities. Most occluders (the black plastic eye cover used during vision testing) have a fold-down pinhole device for this purpose.
A quick and easy way to determine whether refraction is the culprit, short of actually testing different lenses, is with the pinhole test. Punch a small hole in a paper card, and have your patient reread the eye-chart while looking through this pinhole. This can actually improve vision by several diopters. It works because the paper blocks most of the misaligned rays that cause visual blur, and allows the central rays to focus on the retina. If your patient shows no improvement with pinholing, start thinking about other visual impediments like cataracts or other media opacities. Most occluders (the black plastic eye cover used during vision testing) have a fold-down pinhole device for this purpose.
Near Vision
Near vision can be assessed with a near-card or by having your patient read small print in a newspaper. Don’t try using the near-card to estimate distance acuity as distance vision is quite different than close-up acuity. That 20/20 marking printed on the near-card only checks “accommodated” near-vision. Remember that older patients can’t accommodate well and need a plus-power lens (reading glasses) to help them read the card. Carry a +2.50 lens with you when seeing older inpatients as most of these patients leave their reading glasses at home. We’ll cover accommodation and presbyopia in greater detail later in the optics chapter.
Pupils:
The pupils should be equally round and symmetric with each other. You can test reactivity to light with a penlight, but a brighter light like the one on the indirect ophthalmoscope will work much better. When testing the eyes, you will see a direct constriction response in the illuminated eye, and a consensual response in the other eye. These should be equal and synchronous with each other. Also, check the pupils with near-vision, as they should constrict with accommodation.
The Swinging Light Test
 If one eye is injured, or not sensing light, then your patient may have an APD or “afferent pupillary defect.” Often these defects are only partial, making them difficult to detect on casual examination. To detect small APDs, you need to perform the “Swinging Light Test.” Here’s how it works:
If one eye is injured, or not sensing light, then your patient may have an APD or “afferent pupillary defect.” Often these defects are only partial, making them difficult to detect on casual examination. To detect small APDs, you need to perform the “Swinging Light Test.” Here’s how it works:
When you shine a light back and forth between two normal eyes, you’ll find that the pupils constrict, then dilate a fraction as the light beam passes over the nose, and then constrict again. As you go back and forth you’ll see constriction, constriction, constriction, and constriction.
Things look different if one eye is partially blind. As before, when you shine the light in the good eye there is constriction. But, when you cross to the other bad eye, both eyes seem to dilate a little. The bad eye still senses light and constricts, but not as well. So you see constriction, dilation, constriction, and dilation. This phenomenon is also called a Marcus Gunn pupil.
Pressure:
We measure pressure by determining how much force it takes to flatten a predetermined area of the corneal surface. There are several ways to do this and in the ophthalmology clinic we use the “Goldman Applanation Tonometer” that is attached to the slit-lamp microscope.
In the ER, or with patients who are difficult to examine, we can check pressure using a handheld electronic Tono-pen. This little device can be tricky and in the wrong hands becomes a random-numbers generator. I’ll talk more about pressure and its importance within the glaucoma chapter.
Confrontational Fields:
All patients should have their visual fields (peripheral vision) checked. A patient may have great central vision, with perfect eye-chart scores, but suffer from “tunnel vision” resulting from neurological diseases or glaucoma. Your patient may not even be aware of this peripheral visual loss if it has progressed slowly over time.
Confrontational fields are easy to perform but keeping your patient from “cheating” may be tougher. Have your patient cover one eye, and tell them to look straight at your nose. While fixating on your nose, have them count your fingers as you flash them in different quadrants. Be sure to cover your own eye and hold your hands equidistant between you and the patient. This gives you a better idea of what your patient ought to be able to visualize. If you can see your fingers, your patient should be able to see them as well.
EOMs (extraocular movements):
Check extraocular movements by having your patient follow your fingers into all quadrants. If the patient has decreased mobility in an eye from nerve paralysis or muscle entrapment, you may notice this from casual inspection or by more sophisticated cover/uncover tests. More often, though, you won’t see anything but your patient will, complaining of double vision.
Seeing Double?
When evaluating double vision, you must first determine whether the doubling is monocular or binocular.
If, after covering an eye, the vision stays doubled, you know you’re dealing with monocular diplopia. Monocular diplopia isn’t a neurological problem, but likely from a refractive error such as astigmatism, cataract, or corneal surface wrinkling.
Binocular diplopia indicates a misalignment between the eyes … and this is likely due to neuromuscular paralysis or muscle entrapment (if after trauma). To tease out what muscle groups and nerves are involved, you should determine what gaze direction improves and worsens the doubling. We’ll discuss cranial nerve palsies in greater detail in the neuro chapter.
The Slit-Lamp Exam:
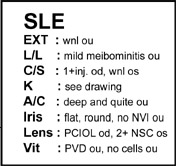 It takes several months to get good at using the slit-lamp microscope. A lot of pathology can be found under the microscope and it’s easy to miss crucial findings. This makes it important to keep yourself organized and describe your findings in the same order with every patient, starting from the outside skin and working your way to the back of the eye. Here’s how we do it:
It takes several months to get good at using the slit-lamp microscope. A lot of pathology can be found under the microscope and it’s easy to miss crucial findings. This makes it important to keep yourself organized and describe your findings in the same order with every patient, starting from the outside skin and working your way to the back of the eye. Here’s how we do it:
External Exam (EXT):
With the external exam, make sure the eyes look symmetric and that the patient doesn’t exhibit ptosis (drooping of the eye) or proptosis (extruding eyes or “bug-eyes”). If the patient has a conjunctivitis, check for a swelling of the pre-auricular nodes (in front of the ear) and sub-mandibular/mental nodes.
Lids and lacrimation (L/L):
Always look at the lid margin and lashes for signs of blepharitis. Evert the lids to look for follicles or papillary bumps on the inside of the lids that might indicate infection or irritation.
Conjunctiva and Sclera (C/S):
Check to make sure the sclera is white and non-icteric, and the conjunctival blood vessels aren’t injected (red and inflamed). If they are injected, see if the blood vessels blanch when you dilate the patient with phenylephrine.
Cornea (K):
Look at the corneal surface for erosions and abrasions that might indicate trauma. Does the stroma look clear? Look at the back endothelial surface for folds or gutatta bumps. Fluorescein dye will make surface abrasions easier to spot.
Anterior Chamber (AC):
Look for cell and flare, which could indicate inflammation or intraocular bleeding. Individual cells are hard to see – you need to turn the lights down and shoot a “ray of light” into the eye. If you compare this light to a projector beam at a movie theater, then “cells” will look like dust flecks while “protein flare” is diffuse and looks like smoke floating in the aqueous. Also, comment if the anterior chamber is deep and well-formed, or shallow and thus a setup for angle-occlusion glaucoma.
Iris (I):
Make sure the iris is flat and the pupil round. If the patient has diabetes or an old retinal vascular occlusion you should comment whether you see any signs of neovascularization of the iris.
 Lens (L):
Lens (L):
Is the lens clear, or hazy with cataract? Are they phakic (they have their own lens), pseudophakic (prosthetic lens), or aphakic (no lens at all)?
Vitreous (V):
You can look behind the lens into the dark vitreous cavity. If you suspect a retinal hemorrhage or detachment, you may see cells floating here.
Fundus Exam:
The fundus is the only place in the body where you can directly visualize blood vessels and nerves. In our notes we typically comment on four retinal findings:
- Macula – Does it look flat? Is there a good light reflex off the surface?
- Vessels – Any signs of AV nicking? Attenuation of the arterioles?
- Periphery – Any lattice, cobble-stoning, or tears?
- Disk – What’s the cup-to-disk ratio? Do the rims look pink and healthy?
You’re probably going to be terrible at the retina exam during your first few months, but do your best. There are several methods we use to view the retina:
The Direct ophthalmoscope
For non-ophthalmologists the most common way to examine the fundus is with the direct ophthalmoscope. This hand-held device is not easy
to use, especially in an undilated eye. The key to success with this instrument is to get yourself as CLOSE to the patient as possible.
Get really close! Dilating the eye also helps.
 Using that darn direct scope
Using that darn direct scope
Switch the light to the highest setting, and rotate the beam to the medium-sized round light. I set my focus ring to “0,” but you may need to adjust this to compensate for your own refractive error. Place your hand on your patient’s shoulder or head.
Starting far away, find your patient’s red-reflex and follow that reflection in as you close in to the eye. Be sure to switch eyes so that you don’t end up face-to-face with the patient (unless they are extremely attractive and you remembered to brush your teeth). Just kidding.
It may take you a while to visualize the fundus with the direct scope, especially in undilated eyes, because the field-of-view you get is very small, making it hard to even recognize what you are seeing.
I find it easiest to find a blood vessel and then follow this vessel back to its origin at the optic disk. Inspect the disk margins and the size of the disk cupping. You may be able to pick up AV nicking from high blood pressure and retinal hemorrhages in the form of dot-blot spots or flame hemorrhages.
At the slit-lamp
The best way to look at the posterior fundus in magnified detail is with a lens at the slit-lamp. This is how we look at the optic nerve and macula in the clinic, but it takes practice. We use smaller, more powerful lenses such as a 90-diopter lens.
The Indirect Ophthalmoscope
This is how we look at the peripheral retina in the ophtho clinic. The eye needs to be dilated to get a good image, but the field of view is excellent. We use a larger, 20-diopter lens, for this.
Other Tests Specific to Ophthalmology:
There are many other exam techniques specific to ophthalmology such as gonioscopy and angiography that you probably won’t be exposed to unless you go into the field. I’ll cover these topics in later chapters as they become relevant.
PIMP QUESTIONS
1. What are the three “vital signs of ophthalmology” that you measure with every patient?
Vision, pupil, and pressure. Some ophthalmologists might say there are five vital signs (adding extraocular movements and confrontational fields.) It’s important to check these signs prior to dilation as dilating drops will affect these measurements.
2. What is a Marcus Gunn pupil?
This is simply an APD (afferent pupillary defect). These usually occur with optic nerve/tract lesions or infarcts.
3. How do you perform the swinging light test?
You shine a light back and forth between the pupils. You should see “constriction-constriction-constriction-constriction” as you flip-flop between the eyes. If you see constriction-dilation-constriction-dilation, then something’s wrong (you’ve discovered an APD).
4. What is “pinholing” a patient?
This is the use of a pinhole to decrease the effects of refractive errors causing visual blurring. When patients significantly improve with the pinhole, they probably need new glasses.
5. When presented with a complaint of “double vision” what is the first thing you should determine?
Whether the doubling is binocular or monocular, as this distinction will completely change your differential. Monocular diplopia is a refractive error while binocular diplopia is a misalignment between the eyes (and a major headache to figure out the cause – see the neuro chapter).
6. What is cell and flare?
These are descriptive terms to describe inflammation in the anterior chamber. Flare is protein floating in the aqueous that looks like a projector beam running through a smoky room. Cells are individual cells that look like dust-specks floating through that same projector beam of light.
7. You are thinking of starting eyedrops to control the eye pressure in a newly diagnosed glaucoma patient. What medical conditions might you ask about before initiating therapy?
Eyedrops can create pretty impressive systemic side effects as they bypass liver metabolism and are absorbed directly through the nasal mucosa. Be sure to ask your patients about heart problems and asthma before starting a beta-blocker.
8. List the eight structures/areas that we check on the slit-lamp exam.
The slit-lamp exam can be intimidating for the novice student, as there are many structures within the eye that we comment on within our notes. Working our way from the front to the back of the eyeball, these include:
EXT (external structures)
LL (lids and lacrimation)
CS (conjunctiva and sclera)
K (cornea)
AC (anterior chamber)
I (iris)
L (lens)
V (vitreous)
You may want to check out the first video, “History and Physical” at Ophthobook.com – in the last half of the lecture I show real slit-lamp microscopy videos and go through this list of slit-lamp findings.
9. Name the four structures we describe in the retina.
The four structures we examine are:
M (macula)
V (vessels)
P (periphery)
D (disk)
I use the mnemonic/acronym “MVP” (Most Valuable Player) to help me remember these.
10. What is accommodation?
This is when the lens changes shape, allowing the eye to focus on near-objects. With age, the lens hardens and we gradually lose our ability to accommodate. We’ll cover this topic in the optics chapter, but I wanted to bring it up in order to emphasize the need for checking both near and far vision during your exam.
I am looking for the information like this!!Thank you
Great book…and very helpful. The author clearly knows what he’s talking about.
please call me about about setting up a web site for by business thank you I will pay you for your services
I have a question related to visual acuity if you have 20/25+3 what does that mean for your visual acuity measurement?
To corinne,
about Ur question…… answer is….he can see 20/25 & 3(letters) from next line of chart but not 20/20 !
also if he see 20/25 except 3(letters) written as 20/25-3
Hend
genior resident
This is an awesome book, very amazing, highly helpful
please give me detail FUNDUS diagram drawing with colors. Thanks
its so helpful and explained in uncomplicated way.thank you and hoping for more topics to be featured..from uae
love the jokes!
thank you sooo much,i looked everywhere for that,thanks!
Well I bypass Daz eye corneal lens discomfort hard to use, except there a way to use lens is hard for me. Can I use the LASIK or not I thank you
nice iam starting to love ophthalmology from this site
Thank you! i have to give the course on ophthamology this year. I have a feeling this will be GREAT 🙂
is there nothing on UVEITIS? we covered that and im wonderng if you wrote abt it
very good i have alot of knwoldge from this topic
thanks alot
Thank you.This site has opened my eye to starting my own blog and informing the public about how to protect their eyes. http://lucentvision.wordpress.com. please visit and comment.
OPHTHOBOOK.COM IS LIKE “A TEACHER IN A LAP”, REALLY.
Wow, ophthalmology is my kind of bite-sized pieces – hallelujah!
thanx alot sir for ur great work
really this is great job ,,,thanks
Just to let you know that I appreciate you having Ophthobook online. Thank you for having this info. free. As a first semester Ophthalmic Student I cannot afford to buy additional supplies to aid me.
While in class sometime I do not understand some stuff and the first thing I do is get on your website where information is always explained in a way that I can understand.
What about the visual acuity, visual fields and red reflex… My professor is obsessed about it!
Would you please make a video about it Doctor? 😀
PS. I love you (I am NOT gay BTW).
Found this sight very beneficial and helpful with E&M auditing and the 1997 eye examination. Do you have a special site or book or other recommendation in regards to the various abbreviations that are utilized and not common in most medical abbreviations books?
Thank you for sharing your knowledge. God bless you and AMERICA!
thank you very much.even after practising as ophthamologist for over twenty years i found this book precise informative and very useful.
gr8 book
thanks sir
Thank you doctor, for making me decide on Post Graduate Course. I was not sure about ophthalmology till I visited your site. Thank you doctor for making me a future Ophthalmologist.
Thank you doctor for being there for making Ophthalmology so interesting and uncomplicated.
Dr. Swarnima Basu
Junior Doctor
i’m a future EM doc and am doing a chill ophtho rotation, this was so good I just bought the book on amazon! thank you
Very good website.
Please update and place more lessons.
It is very good, if you can prepare the step of learning ophthalmology (Schedule for the whole year end). It means what the first year resident should start to read/know, next what to read/do.
Thanks.
Best regards,
When a patient can see the light but cannot track it, is there something wrong with the eye?
Thanks.
Tim Root: Yes. Unless you’re talking about religion.
just love it
simple, easy to understand…
🙂
I practice Family medicine, and I saw the lecture on anatomy of the eye, very great
I apprentice your input for free
I cannot thank you enough for the plethora of information, as if the abbreviations weren’t enough, and now you have provided all this HPI information too. Yes, it is very easy to understand. Call me one happy transcriptionist.
Do you do Ortho too?? lol
really nice presentation.looking 4 material like this
I enjoyed your website information on the eye exam. The information is easy to understand and I appreciate the bit of humor you add. Thank you for taking the time and effort.
Incredible – your book is a lifesaver from all the mediocre MDs out there who think their MD degree automatically came with a pedagogy license!
Easy & gud notes 4 Ophtho Students
What does is mean by “fundus not visualized”? Is this a normal or abnormal finding?
hi there. just wondering, what does ATs stand for under the meds section of the sample note? (page 10)
Thank you so much for providing all this content for free Dr. Root. I’m currently rotating in Opthamology and your teachings are very VERY helpful. You have a teaching gift 🙂
thank you so much for your book. it really helps
the mark of a good teacher is simplifying complicated material in way thats easily understood and remembered, Dr Root does exactly this. thank u so much. never felt so interested to study opthalmology.
THANK YOU SO MUCH. You are amazing DR. Root.
Fantastic resource! Makes a difficult topic easy to understand. Thank you very much!!!
thank u its nice
Awesome resource!! you’re amazing Doctor!! very useful for my ophthalmology clinical posting..
Thank you very very much’ how you have tried to help medical students who are interesting to learn opthalmology
It takes a lot of seflessness to give this kind of resource for free…..you are the man
i am writing to find out that when someone goes to an eye Dr for an exam and their eyes are worse,do the numbers usually go up or down.I am wondering as my husband’s eyes are worse and last time the one said 625 rt eye and 525 lt eye.now his new script says 575 rt eye and 400 left eye. is that possible or are those numbers an indication of the eyes getting worse? my number is 7169900134/ we cannot afford to go order glasses to find they are wrong. thank you.
from candy
pls,cn any one help me out for more easy and uncomplicated books like this…for ent medicine n surgery
loved a lot most easy useful n worthy ..thanks a lot dr root
awsome great job
This is SO helpful! I’m a tech in training coming from optometry to ophthalmology and this video helped me understand much better!
I started loving ophpthalmology after stumbling upon this site.
thanks man love you too.
Thank you
this is what i was looking.
thanks.
i need more information about fundus.
thanks again.
The swinging light test makes so much sense now. I was always curious why the optometrist would shine those bright lights in your eyes. Obviously they are testing for something, but it’s good to now know what it is they are looking for and watching.
you are just awsome
Thank you for a job well done.
Thank you so much for all the time and energy used to put all this together for all of us who have interest in Ophthalmology. You made things easy to understand. Comprehensive, structured and practical. Well done!
P.S. How can I avoid the allocation of an ugly icon to my comment?… 🙂
I really loved this. It was very helpful
Very well done. Thank you!!
4th year med student
Wow. Thanks a bill