Chapter 5: Eye infections
The eye is well protected from infection by the conjunctiva and the corneal epithelium. In addition, the tear film contains antimicrobials while the tear flow itself tends to wash away pathogens. The eye also harbors a host of non-pathogenic bacteria that competitively prohibit new bacteria growth. However, these eye-defenses can be breached by trauma, improper tearing, or contact lens wear and lead to an infection. An eye infection not only threatens vision, but the orbit can act as an entry portal to the rest of the body and infections can progress to systemic involvement, meningitis, and even death.
You will see a lot of conjunctivitis, blepharitis, and corneal ulcers in an ophthalmology walk-in clinic. Here’s a review of the common, less common, and potentially devastating infections you should know about.
Pink Eye: the three types of conjunctivitis
The conjunctiva is the semi-transparent skin covering the white part of the eye. This layer protects the eye from foreign bodies, infections, and irritants. However, the conjunctiva itself is susceptible to irritation and infection from virus and bacteria. Conjunctivitis, or “pink eye,” is the term used to describe inflammation of the conjunctiva and commonly occurs from three different sources: viral, bacterial, or allergic.
 1. Viral conjunctivitis is the most common type, making up half of all cases of conjunctivitis in the adult. It is usually caused by an adenovirus, often following an upper respiratory infection or cold. Viral conjunctivitis is quite contagious and other family members may also complain of having “red eye.” Infected patients typically present with eye redness and watery tearing, but little mucous discharge. Often, only one eye is infected, but the infection may hop to the other side before the end. Two specific signs on exam are enlarged follicular bumps on the inside of the eyelids (these look like tiny blisters) and swelling of the preauricular node located in front of the ear. Most of these infections clear up on their own within a few days. Like the common cold, treatment is geared toward relieving symptoms. Viral conjunctivitis is so contagious that I also recommend good hygiene and no towel/makeup sharing in the home. A lot of people at our hospital present with pink-eye, and this diagnosis is often an instant three-day vacation from work as we don’t want to spread the infection to patients.
1. Viral conjunctivitis is the most common type, making up half of all cases of conjunctivitis in the adult. It is usually caused by an adenovirus, often following an upper respiratory infection or cold. Viral conjunctivitis is quite contagious and other family members may also complain of having “red eye.” Infected patients typically present with eye redness and watery tearing, but little mucous discharge. Often, only one eye is infected, but the infection may hop to the other side before the end. Two specific signs on exam are enlarged follicular bumps on the inside of the eyelids (these look like tiny blisters) and swelling of the preauricular node located in front of the ear. Most of these infections clear up on their own within a few days. Like the common cold, treatment is geared toward relieving symptoms. Viral conjunctivitis is so contagious that I also recommend good hygiene and no towel/makeup sharing in the home. A lot of people at our hospital present with pink-eye, and this diagnosis is often an instant three-day vacation from work as we don’t want to spread the infection to patients.
2. Bacterial conjunctivitis presents with a mucupurulent (pus) discharge. This creamy discharge may cause your patient to complain of sticky eyelashes, with patients finding their eyes matted shut upon waking in the morning. Bacterial conjunctivitis often develops a papillary conjunctival reaction (red bumps on the inside of the lids) and, unlike viral infections, typically does NOT have preauricular node enlargement.
The most common culprits are staph and strep, although with children you should also consider Hemophilus influenza bacteria. In addition, sexually active adults may harbor chlamydial and gonococcal infections (especially with severe or sudden discharge). We treat most conjunctivitis with erythromycin
ointment.
 3. Allergic Conjunctivitis: Finally, patients with allergic conjunctivitis present with red, watery eyes. The hallmark symptoms of allergy are itching and swelling. On exam you may see swelling around the eyes that we call “allergic shiners.” Patients often have a history of seasonal allergies and will usually present with other allergic symptoms such as a stuffy nose and cough. Treatment for allergic conjunctivitis involves avoidance of the offending allergens. These patients may need antihistamines, mast-cell stabilizers, and possibly steroids.
3. Allergic Conjunctivitis: Finally, patients with allergic conjunctivitis present with red, watery eyes. The hallmark symptoms of allergy are itching and swelling. On exam you may see swelling around the eyes that we call “allergic shiners.” Patients often have a history of seasonal allergies and will usually present with other allergic symptoms such as a stuffy nose and cough. Treatment for allergic conjunctivitis involves avoidance of the offending allergens. These patients may need antihistamines, mast-cell stabilizers, and possibly steroids.
Pink Eye … what’s causing it?
The cause of conjunctivitis is not always apparent and it’s sometimes impossible to determine the cause. Typically, you treat with cool compresses, Tylenol, and vigorous hand-washing. If you suspect bacteria, you treat with an antibiotic like erythromycin. Pathognomonic symptoms include:
1. Viral: watering, follicles, swollen lymph nodes
2. Bacterial: creamy discharge, unilateral
3. Allergy: bilateral itching and swelling
Blepharitis:
Blepharitis means inflammation (itis) of the eyelids (bleph), specifically the eyelid margin. This condition is a common diagnosis in an eye clinic, with patients complaining of stinging, tearing, and a “gritty” sensation in their eyes. Blepharitis has been classified many ways (seborrheic blepharitis, staphylococcal blepharitis, etc.) but I prefer to distinguish it as either:
A. Anterior blepharitis:
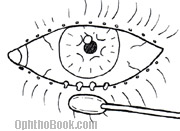
With these patients you’ll find a buildup of debris, or “scurf”, that form as collarets at the base of the eyelashes. Bacteria and irritants live in this debris and constantly shed irritants into the tear film. If severe, you can see small ulcerations and eyelash loss in affected areas.
 B. Posterior blepharitis:
B. Posterior blepharitis:
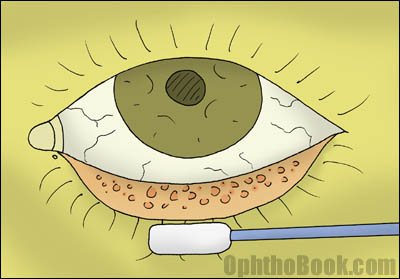
This is when the meibomian gland orifices clog up. When examining the eyelids, I always push on the lid edges with a Q-Tip. If pus-like material oozes out of the pores, then I know that the gland isn’t draining properly. I usually note this in the chart as MGD (meibomian gland dysfunction)
The primary treatment for blepharitis involves good lid hygiene. Most cases can be relieved in a few weeks by having your patient wash their eyelashes daily with baby shampoo and a washcloth. Warm compresses will also help as they open up the orifices of the meibomian glands. Tougher cases of anterior blepharitis may require topical antibiotics. You can also use oral doxycycline – which works not by its antibiotic effect, but by changing the fatty acid oil composition of the meibomian glands, allowing the fluid to flow better.
Blepharitis is common and a large percentage of patients seem to suffer some degree of blepharitis. This is a chronic irritation such that compresses and lid scrub regimens may need to be continued indefinitely.
FUN FACT
In addition to long lashes, camels have an extra eyelid to protect their cornea from blowing desert sands. This eyelid is so thin that the camel can close the lid and still see through it – helpful when traveling through sandstorms.
Chalazion:
 Chalazions are granulomatous inflammations of the meibomion gland. These glands produce the lipid component of the tear film and are deeply located within the supporting tarsal plate of the lid. Chalazions occur when meibomian gland pores become clogged (such as in blepharitis) — lipid backs up into the gland, and a noninfectious inflammatory granuloma reaction occurs.
Chalazions are granulomatous inflammations of the meibomion gland. These glands produce the lipid component of the tear film and are deeply located within the supporting tarsal plate of the lid. Chalazions occur when meibomian gland pores become clogged (such as in blepharitis) — lipid backs up into the gland, and a noninfectious inflammatory granuloma reaction occurs.
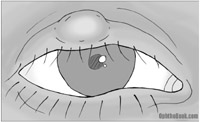
On exam, the patient will have a firm and mobile nodular bump on their eyelid. When you evert the lid, you’ll often see the chalazion bump more clearly. They are non-tender and are not painful.
Early treatment involves warm compresses, massage, and lid scrubs in an attempt to reopen the meibomian pore and allow the material to flow out. If this doesn’t work, we flip the lid and incise/drain the chalazion from the inner eyelid surface. Some people are more prone to developing chalazions and they tend to reoccur.
Chlamydial Conjunctivitis:
Chlamydia causes two different kinds of conjunctivitis: inclusion conjunctivitis and trachoma. Both of these infections are caused by different serotypes of chlamydia bacteria. We don’t see either of these infections often, but they are a major cause of blindness in developing countries.
Inclusion Conjunctivitis:
Inclusion conjunctivitis is the typical “sexual” chlamydial infection of the eye that you’re most likely to see here in the US. Patients present with a chronic conjunctivitis that has persisted for more than three weeks. As with other bacterial infections, the patient will have injection of the conjunctiva and purulent discharge. They may also show follicular “cobblestoning” that develops on the inner eyelids.
This infection occurs mainly in newborns or sexually active teens with a concurrent genital infection. Migration of the bacteria to the eye occurs from hand-eye transmission and can also spread person to person from shared cosmetics or from improperly chlorinated hot tubs. Newborns can also be infected while passing through the birth tract. The bacteria can be detected with a chlamydial immunofluorescence test or by culture of the conjunctiva. A Giemsa stain will show the classic basophilic inclusion bodies within epithelial cells.
Therapy involves topical antibiotics. Because the bacteria is usually contracted sexually, eyedrops alone won’t address the entire problem so oral azithromycin is also given. Sexual partners also need to be treated. Newborns are also treated with systemic erythromycin to avoid chlamydial pneumonitis (chlamydia has a propensity for infecting mucous membranes).
Trachoma:
Trachoma is the “non-sexual” chlamydial infection of the eye that occurs in undeveloped countries with poor sanitation. In less developed countries, trachoma is the leading cause of blindness. The chlamydia bacteria spreads through contact with family members, and can also spread within communities by flies and gnats.
The disease creates a long-lasting, chronic follicular conjunctivitis that eventually progresses to scarring of the eyelids. This scarring can close off the lacrimal gland pores and lead to chronic dry eyes. Scarring can cause the eyelids to rotate inward (entropion), and change the direction of eyelash growth – a condition called trichiasis. Constant rubbing of the lashes against the cornea leads to corneal scarring and eventually blindness.
Gonococcal Infection:
While gonococcal infection is much rarer than chlamydial infection, it is very serious as gonorrhea can progress rapidly. These patients will present with redness of the conjunctiva and profuse mucopurulent discharge. This is a serious infection, as the organism can penetrate through a healthy cornea and perforate within 24-48 hours, leading to endophthalmitis and loss of the eye. The eye can also act as an entry portal for meningitis and septicemia.
 With any severe and profuse exudate you should obtain scrapings and run a culture. A Gram’s stain will reveal the hallmark gram-negative diplococci inside infected cells.
With any severe and profuse exudate you should obtain scrapings and run a culture. A Gram’s stain will reveal the hallmark gram-negative diplococci inside infected cells.
Because the infection advances so rapidly, treatment requires systemic coverage with a drug like ceftriaxone. Topical antibiotics can act as an adjunct but don’t work well alone as the diffuse tearing washes the antibiotic away. If there is severe corneal involvement, or you are worried about your patient’s compliance, you may need to admit them so they can be followed more closely.
Babies can contract gonococcal infection during birth — this is why most states require they receive prophylactic silver nitrate or erythromycin ointment after birth. We use erythromycin here because silver is irritating and creates a temporary “chemical conjunctivitis.”
Corneal Abrasions and Ulcers:
 Corneal abrasions are very common and the most common consult that we get from the ER. Superficial epithelial defects can occur after trauma, infection, or from exposure. The cornea contains more nerve endings per area than anywhere else in the body, so scratches here are painful, and patients will often have photophobia (pain with bright lights) with the sensation that “something is in the eye.” Fortunately, with aggressive lubrication, the superficial epithelial layer heals quickly, literally within a day or two, and the patient feels better. We’ll often treat the eye with empiric erythromycin until the epithelium reforms.
Corneal abrasions are very common and the most common consult that we get from the ER. Superficial epithelial defects can occur after trauma, infection, or from exposure. The cornea contains more nerve endings per area than anywhere else in the body, so scratches here are painful, and patients will often have photophobia (pain with bright lights) with the sensation that “something is in the eye.” Fortunately, with aggressive lubrication, the superficial epithelial layer heals quickly, literally within a day or two, and the patient feels better. We’ll often treat the eye with empiric erythromycin until the epithelium reforms.
If an epithelial defect has an associated bacterial infiltrate, this is called a corneal ulcer. Ulcers are treated aggressively with antibiotics and should be followed on a daily basis until the epithelial defect has closed. For straightforward, small ulcers, we typically use a fluoroquinolone like ciprofloxacin. If the ulcer is large, centrally located, or not healing, then we culture and tailor antibiotics accordingly.
Dangerous Contacts
Contact lens wearers are more likely to have a dangerous infection with pseudomonas. In these patients, we cover with ciprofloxacin. If the ulcer looks bad, we’ll admit for hourly fortified antibiotics (ex. vancomycin and amikacin). Also, we treat any “dirty” ulcer (i.e., caused by tree branch, fingernail, soil) with more aggressive antibiotics.
With sterile epithelial defects you can patch the eye to promote lubrication and speed healing. However, you don’t want to patch an eye with a potential infection and you should follow patched eyes on a daily basis to make sure a perforating ulcer isn’t brewing under that patch.
Pre- and Post-septal Cellulitis:
Patients may present with a swollen eyelid that appears to be infected (swelling, erythema, warmth, systemic fever). When approaching a patient with a taut, infected eyelid the important distinction you must determine is whether the infection is located pre- or post-septally.
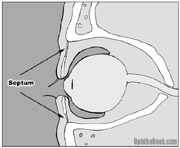 The “septum” is a layer of connective tissue that runs from the tarsal plate of the eyelid to the surrounding orbital rim. Infections superficial to this septum can look bad, but generally resolve without problems. However, if an infection tracks back behind the septum, you’re in trouble and will need to admit the patient for IV antibiotics and possible surgical abscess drainage. Orbital cellulits occurs most commonly from sinus disease, especially in children, with bacteria eroding through the thin ethmoid bone into the orbit. They can also arise from tooth abscess and even from fungal infections in patients that are immuno-compromised with glycemic problems.
The “septum” is a layer of connective tissue that runs from the tarsal plate of the eyelid to the surrounding orbital rim. Infections superficial to this septum can look bad, but generally resolve without problems. However, if an infection tracks back behind the septum, you’re in trouble and will need to admit the patient for IV antibiotics and possible surgical abscess drainage. Orbital cellulits occurs most commonly from sinus disease, especially in children, with bacteria eroding through the thin ethmoid bone into the orbit. They can also arise from tooth abscess and even from fungal infections in patients that are immuno-compromised with glycemic problems.
Symptoms of post-septal orbital involvement are pretty obvious: soft-tissue swelling will cause proptosis and chemosis (swelling of the conjunctiva). Intraocular muscle inflammation causes decreased motility and painful eye movement. If the optic nerve is affected they’ll have decreased vision and possibly an APD.
Whenever you see a big swollen eyelid you should always check for these signs of post-septal involvement and if suspected, order a CT scan. Ophthalmology and ENT has to make this distinction frequently, often in the pediatric emergency room.
Herpes Simplex Virus:
Herpes infection around the eye is quite common – when herpes attacks the cornea, we call this “herpetic keratitis.” Herpetic keratitis is caused by HSV Type-1. This is a common virus, and the vast majority of people contract it during childhood with almost 100% of people over 65 years with latent infection. The virus lies dormant in the trigeminal ganglion and can reactivate, causing cold sores in some people. This reactivation can be triggered by fever, trauma, psychological stress, and UV sunlight. The factors leading to occurrence of the disease at the eye is unclear, though it may have something to do with the virus strain or the patient’s immune system.
 Patients will present with a red, injected eye and complain of pain. Patients may also exhibit the classical vesicular rash near the orbit. The infection almost always occurs in only one eye, though you can see bilateral cases, especially in atopic children. When examining these patients under the slit-lamp, you will see the classic “dendritic ulcer” that stains brightly with fluorescein. The initial infection typically involves only the superficial cornea and doesn’t lead to any long-term sequela. Unfortunately, the infection tends to reactivate. With repeat infections, the virus attacks deeper and deeper areas of the cornea that can lead to scarring if the corneal stroma is involved. Deep infection also kills the sensory nerves of the cornea. This decreases corneal sensitivity (you can check with a cotton-swab prior to anesthetic) and can give patients the false illusion that they are getting better.
Patients will present with a red, injected eye and complain of pain. Patients may also exhibit the classical vesicular rash near the orbit. The infection almost always occurs in only one eye, though you can see bilateral cases, especially in atopic children. When examining these patients under the slit-lamp, you will see the classic “dendritic ulcer” that stains brightly with fluorescein. The initial infection typically involves only the superficial cornea and doesn’t lead to any long-term sequela. Unfortunately, the infection tends to reactivate. With repeat infections, the virus attacks deeper and deeper areas of the cornea that can lead to scarring if the corneal stroma is involved. Deep infection also kills the sensory nerves of the cornea. This decreases corneal sensitivity (you can check with a cotton-swab prior to anesthetic) and can give patients the false illusion that they are getting better.
Treatment is aggressive in order to avoid deeper penetration of the cornea. Debridement of the area with a cotton-tipped swab may help, and topical antiviral drops like Viroptic are always given. Acyclovir is often given orally, and continued prophylactic oral acyclovir may decrease the rate of recurrent outbreaks. I also treat nearby skin lesions with topical acyclovir – this topical drug doesn’t penetrate well into the skin, but may decrease viral shedding into the eye. Topical steroids must be avoided in the presence of epithelial defects, as steroids increase viral replication and can lead to a terrible geographic ulcer on the cornea. With significant corneal scarring, these patients may need a corneal transplant to regain sight.
AIDS and the Eye:
Nearly all AIDS patients develop a condition called AIDS retinopathy, a relatively benign state that is common with CD4+ counts below 200. On fundus exam, you’ll see cotton-wool spots (infarctions of the surface ganglion nerve layer), microaneurysms, and hemorrhaging. The cotton-wool spots are so prevalent that when finding these spots in a healthy patient without underlying diabetes or hypertension you should consider HIV testing. The mechanism behind AIDS retinopathy is unclear, but may result from immune complex deposition in the retinal vessel walls. While AIDS retinopathy doesn’t cause vision problems itself, its continued presence may indicate poor HIV control.
The cytomegalovirus (CMV) is the most common opportunistic infection of the eye and is the leading cause of blindness in AIDS patients. Most people contract CMV during childhood, developing a mono-like illness, and then go on to maintain lifelong immunity with viral suppression. However, the virus can reactivate in AIDS patients because of their decreased immune response. CMV reactivation typically occurs with CD4+ counts below 50; and the overall prevalence of CMV retinitis is rising as better prophylactic treatment for other deadly infections have allowed more AIDS patients to survive with very low CD4+ counts.
CMV typically attacks the retina, and creates a necrotizing retinitis. Fundus exam shows peripheral areas of white retinal necrosis and associated hemorrhaging. The infection is treated with antivirals like gancyclovir or foscarnet. These drugs are only virostatic, though — they will suppress the infection, but won’t eradicate the virus from the eye. Thus, antiviral treatment needs to be maintained to avoid reactivation. The antivirals can be given by IV (you will likely need to admit the patient for gancyclovir induction) with long-term oral maintenance. Also, after induction a gancyclovir implant can be placed inside the eye itself to allow a slow depot release of the drug.
AIDS patients are susceptible to many other eye infections, including herpes simplex of the retina, toxoplasma, zoster, and syphilis. Discussion of these infections is beyond the scope of this book, though, so let’s move on.
Endophthalmitis
Endophthalmitis describes a serious infection inside the eye and is the dreaded complication we most fear after eye surgery. Endophthalmitis is really serious as the eye contains delicate structures and is essentially a large cavity that can quickly turn into an abscess (an eyeball filled with pus). Endophthalmitis can occur for many reasons: after inoculation from trauma or even years after an uncomplicated eye surgery. It can also occur from endogenous infections elsewhere in the body.
While the cause of infection is not always obvious, the infection itself is easy to spot as the eye fills with hazy inflammatory cells and you often can’t view the retina. The anterior chamber inflammation may be so bad that a layer of pus (called a hypopion) forms along the bottom.
Treatment of these patients depends upon their vision … if they see hand-motion or better, we typically perform a “tap and inject.” This is where you put a needle into the eye to draw out a sample for culture and inject broad-spectrum antibiotics back into the eye. If the vision is “light perception” or worse you take the patients to surgery for a vitrectomy to manually clean the eye out. This is only a rule of thumb: the urgency of treatment is also dictated by the cause of infection, such that cataract-induced endophthalmitis is treated differently than glaucoma-surgery induced infection. No matter the cause, however, visual prognosis is universally poor.
Conclusion:
We could discuss many more eye infections, but these are the important entities to know for the wards and your boards. Some of these infections, like blepharitis and corneal ulcers, are very common and you will see these almost daily in an ophthalmology clinic. Others, like gonococcal keratitis and post-surgical endophthalmitis, are rarer, but important to recognize because of their devastating effects if not treated early.
PIMP QUESTIONS
1. A patient comes into your office in great distress because their eye looks incredibly red. On exam, you see they have a spot of hemorrhage under the conjunctiva. Is this a problem and should they be worried?
A few drops of blood spread under the conjunctiva looks impressive and can be alarming. Subconjunctival hemorrhage occurs when a conjunctival blood vessel “pops,” usually after a valsalva or when bending over. This is generally benign as the blood will go away in a few weeks. If the hemorrhage is recurrent, though, start thinking about bleeding disorders.
2. What antibiotic would you use in a small corneal ulcer in a contact lens wearer?
While most small ulcers can be treated with erythromycin, you must worry about pseudomonas in contact lens wearers. Treat all CL wearers with ciprofloxacin or fortified antibiotics if the ulcer is larger.
3. Can you patch an eye to promote healing and comfort? Are there situations where you’d avoid patching?
You can patch an eye with an epithelial defect as patching makes the eye feel better and may speed up surface healing by decreasing exposure. However, you definitely don’t want to patch the eye if there is any chance of infection. Thus, you shouldn’t patch anyone with bacterial infiltrate, contact lens, or trauma by “dirty material” such as from vegetable matter, animals, or dirt.
4. What are the three kinds of conjunctivitis? How do you differentiate them on history and physical exam?
The cause of a conjunctivitis is not always obvious. Generally you’ll see the following classic findings:
Viral watery discharge, follicles, enlarged nodes
Bacterial mucous discharge, often unilateral
Allergic bilateral itching and swelling
5. What’s the most common cause of conjunctivitis? How do you treat it?
Viral conjunctivitis, usually caused by adenovirus, is the most common cause of pink eye in the adult. Adenovirus also causes cold symptoms (rhinovirus actually causes the majority of colds) and these patients will often describe concurrent respiratory illness. You treat these patients supportively with cool compresses, Tylenol, and chicken soup. Warn the patient that they are contagious and encourage them to wash their hands, don’t share towels, and throw out their makeup.
6. What’s our favorite diagnosis in the eye-clinic (good for explaining chronically irritated, grainy-feeling eyes with stinging and occasional watering). How do you treat it?
This sounds like blepharitis, which, along with dry eye is probably the most common diagnosis in an eye clinic. You treat blepharitis with artificial tears, warm compresses, and lid scrubs. If this doesn’t seem to be working, you can try oral doxycycline (don’t use in kids or pregnant women).
7. What’s a chalazion, stye, and hordeolum? How do you treat them?
A chalazion is a non-infectious granulomatous inflammation of a meibomian gland sitting in the tarsal plate (see the anatomy chapter). A stye is like a pimple at the lid margin, usually at the base of an eyelash. A “hordeolum” is a general term that describes an “inflamed gland.” It is debatable what this means, so I don’t like to use the term myself but you may run across it.
8. What are the signs/symptoms of herpetic keratitis? How do you treat?
The hallmark of herpetic infection is the classic dendritic ulcer. You treat with oral acyclovir and topical antiviral drops such as Viroptic.
9. You suspect a patient of having a herpetic corneal infection, based on the shape of her epithelial defect, and you are concerned about corneal scarring. Can you use a steroid to decrease inflammation and the resulting scarring?
You should NEVER use a steroid drop in herpetic disease if there is still an epithelial defect, as this will cause the virus infection to worsen and develop into a terrible “geographic ulcer.” You use topical antivirals like Viroptic and oral acyclovir and wait until the epithelium has healed before considering steroids.
10. Are eyes with herpetic keratitis more or less sensitive to touch?
These eyes are less sensitive to touch as the virus kills the corneal nerves. When HSV is suspected, we check corneal sensitivity with a q-tip or a monofilament prior to anesthetic. Eye sensitivity is an important component of the protective blink reflex.
11. What’s the difference between a corneal abrasion and a corneal ulcer?
A corneal ulcer is an abrasion PLUS an infectious infiltrate. Ulcers require antibiotic coverage and possible culturing depending upon the severity, size, and location of the lesion.
12. A 21 y.o. man presents with a grossly swollen eyelid – a few days before he had a pimple that his girlfriend popped with finger nail clippers. Since then his eyelid has swollen, with redness, mild warmth and tenderness to touch. What specific findings would make you concerned for deeper involvement.
This patient sounds like he has an infection of the eyelid. The question is whether he has any post-septal involvement (i.e. orbital cellulitis). You need to check for decreased vision, proptosis, chemosis, decreased eye motion, and pain with EOMs. These findings would suggest a dangerous orbital infection with the need for admission, imaging, abscess drainage, etc..
13. You are considering doxycycline therapy for a patient with blepharitis. What should you warn your patient about this medication?
Doxycycline is not the easiest medication to take! It is inactivated by milk and your patient may be more susceptible to sunlight and be more prone to sunburn. This medication shouldn’t be used in children or breast-feeding women. Finally, tell your patient to avoid using it at bed-time – the tablet can get caught in the esophagus or stomach and ulcer through overnight.
I am loving this website. Keep it up
This is a fantastic website and a great introduction to ophthalmology! I wish there were more user-friendly (and med-student friendly!) websites like this out there. Would make studying for finals a lot easier.
Thanks a bunch. We spent hours only to look up this topic!
My father had cataract surgery. His vision tested fine immediately afterward, but 3 days post surgery, he was blind due to an infection. Treatment ensued as for endophthalmitis, but he has lost 90% of his vision. He followed all post-op procedures as prescribed. He had the left eye done previously with no problems and is very healthy. I understand from my mom, that the bacteria is Streptococcus. How would he have gotten such an infection? How long would it have taken the bacteria to grow to the point of becoming blind? We believe the infection was introduced during the surgery. His treating physician now says he will never regain his sight as the blood vessels in the eye have dried up.
i lova this book .i am gain valuabul subject
this is great! makes understanding Ophthalmology so much EASIER! keep up the amazing work! 🙂
What about swelling above and below the eye with watery blisters low, just over and below the orbital ridge.
What causes these and what can be done to clear them up?
Thanks,
Janet
what eye drop should be used in contact with allout (parathion)
THIS IS THE BEST WEBSITE….ITS VERY IN INFORMATORY…I LUV IT HAD ALL ANSWERS 2 MY QUESTIONS
I think I got an eye infection from my pet rabbit. He has one and is being treated for it. Upon researching this subject I am highly alarmed at how contagious these things can be!! I think this subject needs to be covered by you.
Tim Root: Hmm … rabbit infections? Well, I don’t think this will make the book, because I’ve never seen a single rabbit-infection in my office … ever. But, I may include a section on the site because it’s interesting. Thanks for writing!
My one year old son has had bacterial pink eye for 10 days now. We have been treating with an antibiotic eye drop the pediatrician prescribed, but his inner eyelids are still super red. I plan on taking him back to the doctor, but just do not understand why it isn’t clearing up.
Tim Root: Melissa, it is often hard to determine the cause of a conjunctivitis (pink eye), especially in kids. This may not be bacterial at all … but a viral infection or allergic response. If viral, it can take several weeks to clear (and the antibiotic won’t make a difference). If allergic, then both eyes are likely involved and this can take even longer. Finally, your child may be having irritation from the antibiotic itself. With kids, I don’t like taking any chances, so you should followup with an EYE doctor to actually look at the eyes and give you a more definite verdict.
i have got an itchy patch on the upper area of my left eye,under the eye brows since 4 months ,i have applied (refresh liquigel,neph-m,gatifloxacin,add tears) anti bacterial,lubricant dry eye drops,but they did not help. even a bit,please suggest something
Tim Root: Kamla, I typically associate itching with an allergic response. It sounds as if you’ve already run through moisturizing and antibiotic drops/ointments. The next step, would be to try an allergy drop. The antihistamine effect will hopefully help with the itching. If this isn’t working, the next step may be to try a short run of steroid ointment to the area. A dermatologist will probably have good suggestions for itching. Finally, you should see an eye doctor or dermatologist to look at the skin to make sure there isn’t something else causing problems, like some kind of small skin lesion.
Ok I noticed my eyes changed over a course of time first the whites of the eye changed tints to slightly darker then I noticed dark circles appeared around the eye.. They water a lot when I’m laying down and are very red early in the morning when I wake up and burn, sometimes I have to rush and use a wash cloth to sooth the burning sensation and get the eye cold out but before I never had any of these problems I also started seeing these small very tiny white bumps appear at the bottom of the eye lids. I went to the eye doc and my eyes were fine no jaundice as well I tested negative for HIV and all hepatitis my eyes just look discolored as far as the white part goes and the dark circles aren’t that bad but I can see them mind you I’m only a 23 year old male.
i been diagnosed with blepharatis gland not draining propley i was told if i use warm compress and clean them with lid care even tried baby shampoo so i have done it as told lift the eye up in lid margin if described right? then was told after time could go back to using make up again treat it like daily cleanseing routine i have for upto 3 times a day, now four months later i still have swollen eye lids and my corneas are red swollen and i havent wore make up was given steriod eye cream from doctor helped but went back to same what can i do sick of not wearing make up and doing what told to only good thing is i dont have pink eye but i do have a swollen eye lids and red cornea help please
I have a lump in coming from the inside of my eyeball, but i also have glaucoma, what could be wrong? Oh yea, wen i touch it thru my eyelid it messes up my vision.
Excellent about anterior segment diseases, If anybody having these problems, must go to an Optometrist/Eye care specialist for diagnosis.
Visit optometrist- (only qualified ) every six months for regular eye check up
Regards
Raju
Optometrist
Optom from AIIMS, FELLOW OPTOM-LVPEI
Odisha-india
I was having unexplained itching in my crotch which I thought to be a yeast infection but later found out it wasnt. Still not sure because I have tested negetive for chlamydia and gonnorhea. No herpe outbreak yet a month later I started itching a dry burning pain in my eye. A week later it is still there. No discharge in the eye when I wake up very painful like glass in my eye and takes a minute to open and see. I went to an optimologyst and he said no sign of herpes thus far. Not sure what this is..now both my eyes hurt and my lower lid is dry and itchy too. Anyone help please..?
Hi. I have a small lump, end of pencil size max, which appears in the top inner corner of my right eye. Feels as though its close to the bone socket area. If Im bending and increase blood pressure with my head down it becomes pronounced and slightly sore. When I stand straight after about ten minutes it goeas away. When it is present opening my eyes wide causes slight pain in the lump area. Been there for about 5 days. Before that had a sore area central between my eyes on the bridge of my nose for couple days. Now ok. Any clues????
hey, i got conjunctivitis about a year ago from sharing makeup, and although my eyes were only red for about two weeks, i still wake up with junk in my eyes and my eyelids are kind of constantly swollen, but not that swollen. only slightly. Ive been to the doctor several times, every time she gives me a prescription, tells me to use it for a few weeks, i do. it works for a while then it just comes back. Do you have any idea what it could be?
I have two very tiny white (ulcer like) bumps on the plate of my left upper eyelid. It itches and feels very sore and I’m really scared that it might not be a stye but something much worse. Please help
i have pain some time my one eye.i used concatc lence but i stop now.after few days my one eye is small then other,plz help
Hello, My eye has been swollen off and on for six days now, its red and itchie , I took benadryal it didnt work, now taking sudafed walgreens brand, and also put corisone for the itching, yes it help doing the day the swelling is in control, but early in the morning my eye is swollenall over , then i have one small bump in the swollen area and it itch.
Please can anyone thats qualified what could this be.
Thanks
What a great web site! I have been misdiagnosed for almost a year and finally saw an EYE doctor. I was prescribed a Prednisolone eye drop, Bacitracin ointment for use at night, and Doxycycline. While I am thankful for medications that are helping so quickly, I now understand why I am having such a terrible time with the Doxycycline. The eye doctor never explained what I have, and when asking about the truly horrible side effects of the Doxycycline that I was experiencing, I was told to “just take it”…..for two months. Glad to understand the eye better as a whole, and not feel “crazy” about my interactions with the oral antibiotics. Btw, for anyone who reads this, I got this really severe and painful infection from eyelash extensions from a reputable and expensive eyelash bar. Please be wary!
72this month and in good health. My are bloodshot red all the time and have been for years. Opthymologist has not been able to find the problem. I have tried many drops, latest Allrex, to fix it. I am embarassed to look people in the eyes because I know how bad mine look. My eyes tear up under strain of reading and computer screen. No bumps, infections, have been diagnosed. I do get headaches because the backs of my eyes are in pain a lot. I feel that as I age this gets worse. I go thru periods of cleaning eyelids during the day. Tried ointments and prescribed drops. In the past they would clear up temoraraly with a steroid drop but I have given up on counting on that. Too dangerous.
I was exposed to defolient in the vietnam but there are no studies on that. Help
very educative and helpful in understanding eye troubles and their basic precautions.
please put a forward link on this website to share info with others
I have been getting eye infections for the last five to six years. I used to wear contact lenses. When I visited an eye specialist, he told me that my infections were due to my contacts as due to my age (56yrs), so he said i should do lasik to correct my vision, which I did, but still i keep in getting these infections, more serious than ever.
I have had two infections since my lasik, which was done in Nov. 2010. What could be the reason. My eye becomes red and quite painful though there is no tearing or any discharge.
really appreciate your website but just wondering, if my sons condition is treatable. he has reddy eyes, watery and constantly has a discharge. hes had problems since birth.please advise
My son is 6 years old and since he was 2 1/2 he has had this TERRIBLE recurring infection of some sort around his eye. We have seen Dr, infectious disease, ophthalmologist, and all seem to have no idea what the problem is. To this date he has had about 10 of these. It starts out as redness around the eye like pink eye, then swelling and eventually the underneath of his eye swells to the size of a golf ball!! Then it starts to get small rashy looking blisters all under the skin of the eye. There is never usually any discharge othewr than watery eyes. They say periorbital cellulitis and did a CAT scan to see if there were any under lying issues, but everything came back fine. I am desperate for an answer!!! I feel so bad for him and do not want him to have to deal with this the rest of his life. Nothing I google seems to look quite like it either. If anyone could help me, I have pictures of this to show exactly what I am describing.
For those of you with unexplained redness and infections, have you been tested for food allergies? I would definitely get the little boy food allergy testing and possibly the 72 year old gentlemen as well. Have the blood testing done. My symptoms got worse and worse and finally after MANY years I was tested and had 24 allergies and a yeast overgrowth. When I eat properly life is good, but when I don’t I get my symptoms back slowly but surely.
I have Crohns disease and I am aware that that can affect my eyes, I now have an eye infection how do I know if it is the Crohns or just an eye infection?
I got a tiny bump on my eyelid liKE a bubble& it make me so uncomfortable like I got somethin in my eye.Dutse, Nigeria.
I have a lump between my eye and nose – not sat on tear ductbut lower down. Looking at anatomy of the nose, its probably sat over the superior turbinate bone area. I’vebhad this for years. No pain. No weeping excep sometmes I knock the end of it and it bleeds (minimal). It sort of resembles a wart – approx .25 x .5 cm. circular and slighty reddened. I ahev looked at lots of internet images but cannot find anything comparable. Thank you.
I also had some trouble related to eyes, I had back pain which led to right hand numbness and face numbness, I went to a neurologist he told go for an MRI I went for an MRI, reports Normal, he gave me anti anxiety tablets, after eating those I started getting more depressed as the numbness continued, I went to an ENT, for a second opinion He was an OLD 75 years old doctor, he saw me and told me, Son did u check ur eyes, I said no, He said go and check, I went to the eye doctor he said you have -2 on both sides and major eye infection he told me wear specks and put eye drops called GENTEAL, Guys I have recovered 20percent in 1 day now the numbness and pressure near the bridge of the eye is minimal and I feel good again. But he never told me what did I have, like what type of infection?
My daughter has an extra row of eyelashes, she used to get chalazions on both eyes and now she has a reoccurring corneal ulcer in her left eye right in front of the pupil. It all started when she was about 4-5 and the ulcer appeared last year when she was 7. We have seen a couple ophthalmologists and a cornea specialist. They have ruled out that it might be a bacterial infection from the chalazions or the herpes virus. She has been put on a couple different antibiotics, steroids and recently a pill for the herpes virus. The drops work to help it get better, but shortly after discontinuing, as she can’t be on drops forever, it comes back. They can’t seem to determine what it is and/or why it keeps coming back. Due to the fact that it’s right in front of her pupil her vision is affected. When it is acting up she can’t see my hand not even 5 feet away from her face. After it gets better, the best she has had is about 20/60. Any help would be greatly appreciated. Thank you.
My now5 year old has been suffering from extreme photophobia (on and and off..mostly on), bumps in her inner eye lids, and swelling around her eyes since she is 10 months old. This all started after she had a corneal abrasion we believe from scratching her eyelids. She has had it all done. Neurologist cleared her, eye docs (everywhere)say actual eyes are fine, allergy tests (about to her a most in depth allergy test today since she just turned 5), mri, ct scans, various blood tests and cultures. They say..”it will burn off”.. This was last thing suggested to me from reputable eye clinic for children. After today, if no results are produced, I have hit a wall and need to start over. I feel like it’s viral but they all tell us no. What are we missing? Any suggestions? Other than this, she goes to school (with blanket on her head to get her into the car)..Very bright, social and has friends. This is hurting the quality of her life and lately appears to be getting worse (why we thought allergies as well but they tell us no still). Could there just be some irritant causing this that we have not found yet?
i learned alot from that cuty i guess he is kim root this site is just MINDBLOWING!!!!!!!!!!!!!!!!!
I have had recurring chalazions for almost 4 years now. I have had cortisone shots and 3 excisions. Almost a year has passed since my last one has been excised and I have another one. This has been recurring in the same eye. I do the eye washes, warm compresses and have used doxycycline and Zylet drops. What can be done at this point? My doctor said if it does return surgery would be needed. What exactly is he referring to and is there anything else I can do? Thanks so much!
I have littel white bumps inside the left eye lid about twenty of them. eyelids right and left slitely burn. can you help thank you.
My four year old could not open his eyes this morning – it was shut by a sticky puss. It had a creamy/yellow colour that I had to wipe off with a warm cloth. what is this and what treatment can I get over the counter for him?
I am a CL wearer and a week ago i noticed some tiny bumps in my conjuctiva(follicles) on both eyes, my eyelids not tender, it doesn’t hurt, no discharges at all and most importantly my eyes not red or pink, they look normal unless you pull down my lower lids and take a closer look of the conjunctiva. I did a culture of the tiny bumps and it was identified as Steno maltophilia. What is this disease or infection am getting? Help me please.. i am worried. Thank you.
This is such a great resource to have available for general usage. Thank you!
Looking for a abscess surgeon, because, I have a lump under my upper eyelids. I think the infections are called, Periorbital cellulites and Orbital cellulites. In other words, “Eye Cyst”….
Thanks,
ph: 240-599-6773
Hello,
My partner has been randomly suffering from a white cloud which appears in her left eye only. It started around 2 years ago and in the last 2 days she has developed it again. This “cloud” is clearly visible for me to see, it is around 1 tenth the size of the eye ball and moves around the whole eye, never fixed in one place. So far, all known eye tests of a basic level have been conducted with no unusual results coming back from the lab. The treatment which she is receiving is a daily injection directly into her eye. She is Russian and her medical vocabulary is basic, hence my basic description. She is receiving her treatment in Russia and I fear this could be a problem. This problem is killing her mentally with no diagnosis been made after all the tests. Please, if you have any advice, anything at all, I would be all ears. Thank you so much in advance.
My eyes have ths strippy watery to white moving cloud around my puple and on the white lining cornea i can still see the liquid movements.this all started 4(four) months back please advise me on my condition and the treatment i should be taking to avoid futher infections or loss of vision.i’ll appreciate your info.thanks
Really nice book like to read it completely.
What is going on systemically that causes chalazions???? I’ve had 2 in the last 4 months and yesterday I had an pus filled area near an eyelash?
hi i am suffering from acute bacterial conjuctivitis and pus discharge from eyes and also formation small tiny granules inside the upper eye lid.. i m using exocin and florozil eye drops but not working
tell any eye drop for this condition
nice work >>>keep it up 🙂
My doctor says I have galcoma. I don’t have infected eyes.
My Pink eye started back in August. all thqtvwas done sine has been different antibiotic drops and steroids. they have not worked. my eye is no longer red tyat was taken care of in sept. but both eyes stings and my right eye vision is horible. has to be bacteria but i dony know what else can be done.
P.s I might add I have it still its my 9th day, and cannot open my eye as it extremely painful 🙁
I have had’conjunctivitis’ on and off for three months now. Have had treatment, but it still keeps coming back. Everytime I go to the walk-in the docotr just says its the same thing, although my kids did not get it repetitively. I am concerned that there is more to this, what are the tests that I should ask them to perform to get results? My eye is so painful it’s causing me headaches at work, and stinging constantly. Then it will subside for a week and then come back… HELP!
I also have continuous problems with conjunctivitis for a while now. I did manage to get some drops straight from the pharmacist called Brolene Eyedrops for mild short term conjunctivitis that I use as soon as I start to get it back and this is keeping it under control and saves the continuous doctors visits.
I am going to try some diet changes and found some good information here in this article if you are interested.
http://healthnewsnetwork.org/how-to-have-healthy-eyes
Should people with any of these problems see a family physician or an eye doctor?
Love this site! You guys covered a wide range of eye issues but, unfortunately I did not come across the information that pertained to my issue. My boyfriend came back from a beach vacation and his eye is severely swollen and there seems to be a water blister on his eyeball? It is very red (bloodshot)he has a lot of pressure behind his eyeball as well. The pressure was the first sign of a problem. This issue has developed very quickly over 2 days. Could it be a parasite of some kind? Is there a home remadedy? He has a specialist appt. but that is in a few days We need help Now! I have gone to just about every site I could think of for the answers
I know this sounds funny but I assure you its real and happens every time no matter where I go to the bathroom to pee my eye’s tear up and it looks like I had cried but not sobbing, just a few well developed tears stream down from each eye and it stops. this has always happened to me for as long as I can remember however I am in no pain during before or after. Have you ever heard of something like this?
Several ppl do this. I don’t know why.
I love this website, I used to hate ophthal until I got hooked onto this website. And dr. Root, you’re awesome!
This is a great site. Love all the information. Thanks
AS A OPHTHALMIC ASSISTANT ITS VERY USEFUL TO REMEMBER ALL THE THINGS IN OPHTHAL.AND A LOVELY WEBSITE.THANK YOU
Please help me, for the past 2 months I have had a white or very pale blister under my right eye it is about 2 centimeters from my actual eye, I have large bags under my eyes and it’s sitting there, today I have another one appeared very close to it. This eye aches very much please could anyone tell me what they are I fear the worst. Thank you so much.
Good morning
My has has been sore for 2 weeks now
It is very itchy, red swollen and has gone smaller than than the other eye. I have used optrex- over the counter medication but that did not work. My doctor prescribed me with fusiphalmic eye drops and that is not working either.
The doctor is so booked up and was offered a appointment for Next Friday. When I woke up in the morning it sometimes be’s sticky and also have noticed a little bump white not red on the croner of the upper eye lid. The inside eye is red- blood shot
I really need help here please. I can send a pic please let me know how. please help
If your eye doctor is that busy, you should go see a different eye doctor to have your eye looked at. This kind of thing can’t, and shouldn’t, be diagnosed online.
Great site ! In here actually to try and find a link between hpv1 infected corneal graft and activation of cluster headaches. I have the cluster ongoing and have recently received a corneal transplant that is opaque.The emergency transplant was due to an uncontrollable corneal ulcer that progressed to perforation! Am grateful to still have the eye (and the chance to regain vision with a new clear graft) but am curious about the reappearance of the cluster headaches after being free of them for 10 years!
Hi,
Can you please advise if you know why i would have an eye infection for 2 years i have gone to an doctor, optician, eye doctor who said it was chronic sinus and then got my sinus done and to be it had nothing to do with my sinus its an infection.
I have used anti biotic drops and anti biotic oral and it has cleared the infection but it re occurs over and over again.
i am now waiting for a specialist appointment.
my is is sore and red all the time and painful sometimes
Thanks for reading my comment!
Can u get pink eye on the bottem of your eye
i was told i have an eye infection called parientitus. i do not think i have correct spelling will you be able to tell me more about this infection or where i can get info about it please
from lisa
Never heard of it. Could it be “panuveitis” or “pingueculitis?”
Can there be a condition where only one eye is affected with bacterial infection ?
It’s always fun learning with you. You’ve helped me come a long way through Optometry school. God richly bless you and your work.